Secondary bile acids from intestinal bacteria promote colon cancer
Researchers at the Technical University of Munich, RWTH Aachen University and the German Institute of Human Nutrition Potsdam-Rehbr├╝cke (DIfE) have experimentally demonstrated for the first time a causal role of microbially formed secondary bile acids in the development of colorectal carcinoma (CRC). The results, published in the journal Gut , link a high-fat Western diet to changes in the gut microbiome and open up new approaches for prevention and therapy.
Colorectal cancer is one of the most common and deadliest cancers worldwide. Genetic factors play a role, but environmental and lifestyle influences in particular determine the risk. A typical Western diet high in fat and meat as well as low fiber intake is closely related to CRC. It alters the gut microbiome and stimulates the production of secondary bile acids by bacteria with 7-alpha-dehydroxylation activity (7╬▒DH-positive bacteria). The dominant secondary bile acid deoxycholic acid (DCA) has long been considered to increase risk, but causal mechanisms have remained unclear until now.
The interdisciplinary team developed models that depict human conditions as accurately as possible. In a genetically modified pig model (APC1311/+) that spontaneously forms colon polyps, a Western diet exacerbated tumorigenesis. Increased epithelial cell proliferation correlated with increasing concentrations of fecal secondary bile acids, especially DCA. The administration of colestyramine, which binds bile acids, reduced this effect and slowed down tumor growth.
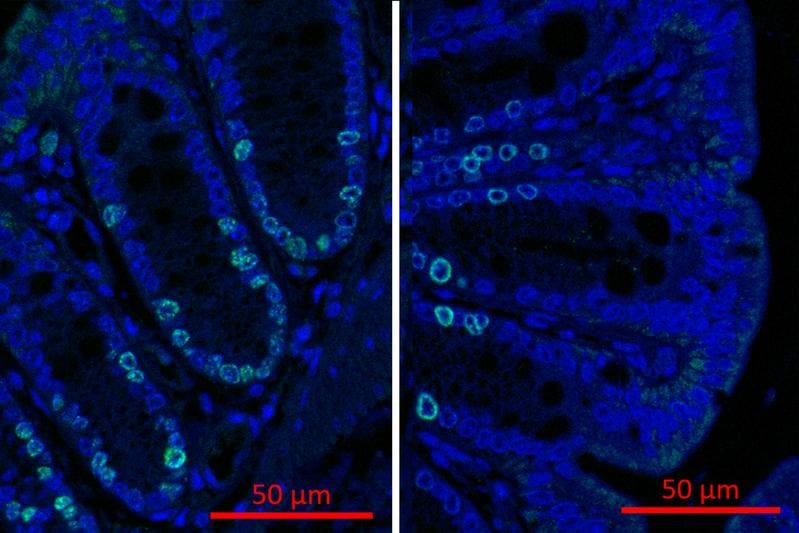
In gnotobiotic mice, which were kept germ-free and specifically colonized with 7╬▒DH-positive bacteria, DCA production triggered an accelerated proliferation of colon epithelial cells. This was shown by increased levels of the proliferation marker Ki67 as well as altered gene expressions affecting cell differentiation. In several CRC models, these bacteria significantly increased the tumor burden, while genetically modified strains without DCA formation capacity had no effect. This proves a direct causal role of bacterially produced secondary bile acids in the development of cancer.
Analyses of stool samples from established human CRC cohorts confirmed the animal findings. Patients had significantly more 7╬▒DH-positive bacteria such as Clostridium scindens than healthy controls. In the future, the specific detection of such bacteria could help to identify at-risk individuals with an unfavorable diet and lifestyle at an early stage. Targeted nutritional interventions could reduce the production of secondary bile acids in them and have a preventive effect.
Primary bile acids are formed in the liver from cholesterol and support fat digestion as emulsifiers. In the colon, specialized bacteria convert them into secondary forms such as DCA and lithocholic acid. The majority circulates enterohepatically, but a small part reaches the large intestine directly and can have a carcinogenic effect there.
The study highlights the long-term impact of a high-fat diet on the microbiome and gut health. Future work should isolate and study additional 7╬▒DH-positive bacteria from different populations to better understand dietary variations. The findings lay the foundation for microbiome- and nutrition-based strategies for CRC prevention, for example through bile acid binding or targeted microbiome modulation.
Original Paper:
Editor: X-Press Journalistenb├╝ro GbR
Gender Notice. The personal designations used in this text always refer equally to female, male and diverse persons. Double/triple naming and gendered designations are used for better readability. ected.




