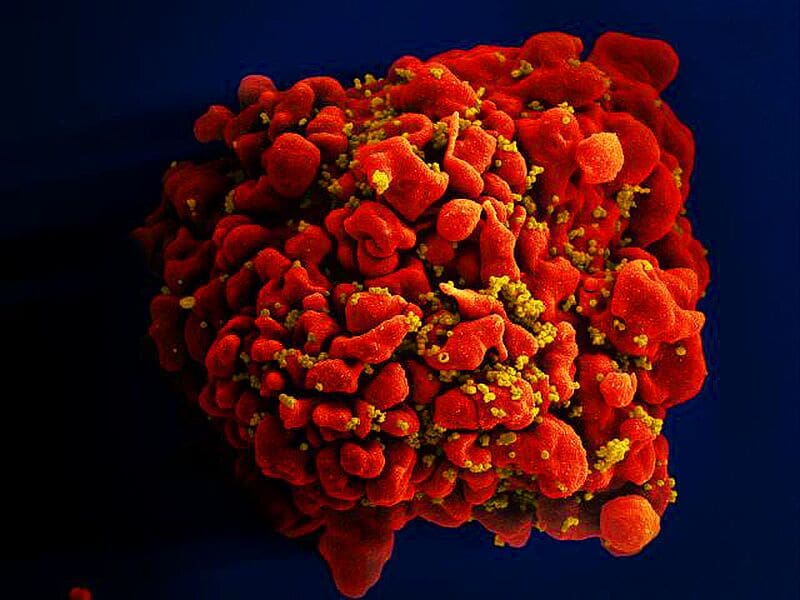
Expert report warns of impending supply bottlenecks in HIV treatment
A report on HIV care in Germany presented yesterday in Berlin sounds the alarm: by 2035, there could be a shortage of up to 130 specialized HIV doctors to meet the growing demand for high-quality care. This corresponds to around 26 percent of the required specialists. Particularly in rural regions, there is a risk of significant access problems, which could make it much more difficult to provide care for people with HIV. The report was commissioned by the German Association of Outpatient Physicians for Infectious Diseases and HIV Medicine (dagnûÊ), the German AIDS Foundation (DAS) and the German AIDS Society (DAIG) and prepared by the IGES Institute in collaboration with the Central Institute for Statutory Health Insurance Physician Care.
High standard, but growing challenges
Germany currently has an efficient HIV care system based on specialized practices and outpatient clinics. Around 80 percent of people diagnosed with HIV are successfully treated by contract physicians with HIV specialization. However, the burden on the system is growing rapidly: between 2014 and 2023, the number of patients in specialized care increased by 38 percent – from 49,500 to 68,500 per year. Assuming a stable rate of new diagnoses, the number of patients is expected to rise to 96,500 by 2035. At the same time, the number of HIV services utilized could increase by 44 percent over the next ten years – without taking into account age-related comorbidities such as metabolic disorders or depression.
However, the number of HIV specialist practices has been stagnating for years. Although a slight increase in the number of practitioners is to be expected, the trend towards larger practices and medical care centers (MVZ) is leading to a concentration of care in metropolitan areas. This exacerbates the problems in rural regions, where patients often have to travel long distances to specialist practices or HIV outpatient clinics. Older people with HIV, whose need for treatment increases due to complex comorbidities, are particularly affected by these hurdles.
Data basis and methodology
The report is based on a comprehensive analysis of contract physicians’ billing data on outpatient HIV care from 2014 to 2023, supplemented by hospital reports, billing data on inpatient care and a nationwide online survey of people with HIV. This data not only shows the current state of care, but also enables reliable forecasts for the coming years.
Recommendations for action to secure the supply
Without countermeasures, there is a risk of structural collapse in HIV care in parts of Germany. The report therefore formulates specific recommendations for action:
- Strengthen the promotion of young talent: Support programs should create targeted incentives for general medical and internal medicine practices to participate in HIV care. Flexible training authorizations could involve more specialist practices, and the expertise at clinical and university centers must be secured.
- Facilitate participation in HIV priority care: Doctors who want to qualify need organizational, professional and financial support. Cross-sector cooperation models can facilitate qualification.
- Avoid gaps in care in rural regions: Telemedicine network models and consultation options should be promoted across the board. In structurally weak regions, transportation assistance could secure care.
- Expand access to prevention: HIV pre-exposure prophylaxis (PrEP) must also be made accessible to previously underserved target groups, supported by permanent extrabudgetary remuneration.
- Expand geriatric and psychosocial care: As patients age, the need for geriatric and psychosocial support increases. This requires better networking, training in care and the involvement of psychosocial specialists – including digitally.
Outlook and availability
The report was presented to the public on July 10, 2025 as part of the HIV 2025 Forum in Berlin. A summary is available online, the full version can be found on the dagnûÊ website.
Read also:
One Health: Climate change worsens HIV prevention – MedLabPortal
Editorial office: X-Press Journalistenbû¥ro GbR
Gender note. The personal designations used in this text always refer equally to female, male and diverse persons. Double/triple references and gendered designations are avoided in favor of better readability.